Lifestyle Medicine Saves Lives
“The greatest wealth is health.”
—Publius Vergilius Maro
If a person is having a heart attack and someone saves their life by performing cardiopulmonary resuscitation, the rescuer, whether they’re a medical professional, firefighter, police officer, or ordinary citizen, should be celebrated as a hero!
They just saved a life!
They just kept someone from dying of a heart attack!
If one of your coworkers walks into your office and sits down to eat their nutrilcious lunch while they chat with you or tells you they just went for an enjoyable swim or run during their lunch hour, they too should be celebrated as a hero!
They just saved a life!
They just prevented a heart attack from happening!
This is lifestyle medicine, the use of evidence-based approaches to nutrition, exercise, stress reduction, and holistic wellness to reverse and prevent sickness and optimize longevity and wellness.
The Future Has Arrived
Lifestyle medicine is the way of the future, and the future has arrived.
People come to me every week and tell me:
“I know I need to do something about my blood sugar, blood pressure, cholesterol, and/or weight. They want to keep throwing pills at me, but I know I can take care of this by improving my lifestyle. That’s what I want to do.”
They often look me right in the eyes and say something like:
“Lifestyle is what got me here; lifestyle is what’s going to get me to a better place.”
It’s hard to argue with that.
Side Problems and Side Benefits
You’re well aware of the fact that most medications come with “side effects”.
“Side effects” is the pretending-to-be-benign term big pharma uses for what are really side problems.
Common side problems of widely taken medications include:
- Fatigue
- Nausea
- Sleepiness
- Sleeplessness
- Pain
- Joint pain
- Muscle pain
- Headaches
- Constipation
- Diarrhea
- Fast breathing
- Shallow breathing
- Cramping
- Sexual dysfunction
- Weight gain
I don’t know about you, but when I think about “effects”, I think about things like mood lighting and background music not nausea, sleeplessness, diarrhea, and cramping.
These are problems—the side problems of medication.
Lifestyle improvement, on the other hand, tends to come with side benefits.
Let’s say you decide to lower your blood-sugar levels via lifestyle improvement. You likely have a very good chance of doing so, and you’re also likely to experience:
- A longer life
- A reduction in risk of a host of other ailments
- Better quality of sleep
- Better digestion
- Higher energy levels
- Higher sex drive
- Better mood
- Higher productivity and income
- Lower lifetime medical costs
- The pride of being a positive example for others including kids
- Empowerment that spills into all areas of your life
With lifestyle medicine, you have the opportunity to avoid side problems altogether and instead enjoy an impressive array of side benefits.
A Potent Approach
Lifestyle medicine is extremely potent.
A large, longitudinal scientific study conducted at Harvard University drives this point home.
The researchers followed more than 123,000 subjects for 34 years. They took various measures of behavior from the subjects and noted which subjects died during that time period and when they died.
What did they find?
“We estimate that adherence to a low-risk lifestyle could prolong life expectancy at age 50 years by 14.0 and 12.2 years in female and male US adults compared with individuals without any of the low-risk lifestyle factors. Our findings suggest that the gap in life expectancy between the United States and other developed countries could be narrowed by improving lifestyle factors.”
The salutary lifestyle they studied (refraining from smoking tobacco, moderating consumption of alcoholic drinks, eating nutritious food, exercising, and maintaining an optimal weight) was worth an average of 13.1 years of life.
That’s more than 4,500 sunrises!
Subjects who lived this salutary lifestyle had an 80 percent lower risk of dying from cardiovascular disease and a 60 percent lower risk of dying from cancer. (1)
The scientific literature about lifestyle medicine makes two things very clear:
- Detrimental behaviors strongly correlate with negative outcomes.
- Beneficial behaviors strongly correlate with positive outcomes.
In a scientific study with results published in JAMA Internal Medicine, subjects who consumed 10 percent more of what the researchers classified as “ultraprocessed food” had a 14 percent higher risk of dying during the time period studied. (2)
Conversely, in a scientific study with results published in The Lancet, each serving of vegetables consumed per day correlated with a three percent reduction in risk of stroke, and each serving of fruit consumed per day correlated with an 11 percent reduction. (3)
In a scientific study with results published in the European Journal of Cardiovascular Nursing, sedentary subjects had a 75 percent higher risk of dying during the time period studied. (4)
In a scientific study with results published in the Journal of the American Heart Association: Cardiovascular and Cerebrovascular Disease, meeting the generally recommended minimum exercise load correlated with a 17 percent reduction in risk of cardiovascular disease and a 26 percent reduction in risk of type-2 diabetes. (5)
I could go on all day with scientific evidence like this. What it all points toward is a very powerful fact that gives you a lot of power:
Your behavior greatly influences your well-being.
Head-to-Head Comparison
Another way to explore the potency of lifestyle medicine is to directly compare it with medication. Lucky for us, a group of researchers did just that and published their results in The New England Journal of Medicine.
The subjects in this scientific study were people with prediabetes. It was a randomized, controlled study with control, lifestyle-intervention, and metformin (a widely taken medication) groups.
The researchers found their lifestyle intervention was more than twice as likely as metformin to prevent a person with prediabetes from developing type-2 diabetes:
“To prevent one case of diabetes during a period of three years, 6.9 persons would have to participate in the lifestyle-intervention program, and 13.9 would have to receive metformin.” (6)
Lifestyle medicine comes without side problems, comes with an impressive array of side benefits, and just plain works.
Lifestyle Medicine Is Holistic
It gets better.
Lifestyle medicine is also holistic.
Salutary behavior knows no bounds. That is, when you do something that meets one or more of your needs, it helps you experience better physical, emotional, and mental wellness.
For example, in a scientific study with results published in The Lancet Psychiatry, exercisers reported 43 percent fewer days of poor “mental health” than nonexercisers. Here’s how the researchers summarized their findings:
“In a large US sample, physical exercise was significantly and meaningfully associated with self-reported mental health burden in the past month. More exercise was not always better. Differences as a function of exercise were large relative to other demographic variables such as education and income. Specific types, durations, and frequencies of exercise might be more effective clinical targets than others for reducing mental health burden, and merit interventional study.” (7)
Similarly, behaviors often considered more emotional or mental in nature have tangible effects on outcomes often considered more physical in nature.
For example, in a scientific study with results published in PLOS Medicine, people in stronger relationships were 50 percent less likely to die during the time period studied compared with people in weaker relationships. Here’s how the researchers summarized their findings:
“Data across 308,849 individuals, followed for an average of 7.5 years, indicate that individuals with adequate social relationships have a 50% greater likelihood of survival compared to those with poor or insufficient social relationships. The magnitude of this effect is comparable with quitting smoking and it exceeds many well-known risk factors for mortality (e.g., obesity, physical inactivity). These findings also reveal significant variability in the predictive utility of social relationship variables, with multidimensional assessments of social integration being optimal when assessing an individual’s risk for mortality and evidence that social isolation has a similar influence on mortality to other measures of social relationships. The overall effect remained consistent across a number of factors, including age, sex, initial health status, follow-up period, and cause of death, suggesting that the association between social relationships and mortality may be general, and efforts to reduce risk should not be isolated to subgroups such as the elderly.” (8)
Your body, heart, and mind are inextricably linked. They are one. As such, whenever you proactively meet one of your needs, you’re better off—physically, emotionally, and mentally.
Wellness: It’s holistic.
Lifestyle Medicine and Genetics
Lifestyle medicine also trumps genetics.
In most cases, how you live has a much greater impact on your well-being than genetic predisposition.
Consider cancer and dementia, ailments many people think of as ailments that just happen. Many people think there’s little that can be done to prevent cancer and dementia.
A tsunami of emerging scientific evidence tells a different story.
Regarding cancer:
“The fact that only 5-10% of all cancer cases are due to genetic defects and that the remaining 90-95% are due to environment and lifestyle provides major opportunities for preventing cancer. Because tobacco, diet, infection, obesity, and other factors contribute approximately 25-30%, 30-35%, 15-20%, 10-20%, and 10-15%, respectively, to the incidence of all cancer deaths in the USA, it is clear how we can prevent cancer.” (9)
Regarding dementia:
“Assuming that risk factors do not operate independently, approximately 48.4% of dementia cases in Australia can be potentially attributed to midlife obesity, physical inactivity, smoking and low educational attainment. Any intervention that reduces the prevalence of these by 5%, 10%, 15% or 20% per decade can have a significant public health impact, especially with regards to lowering the direct and indirect costs incurred by both governments and those living with the disease. Further research is needed which aims to provide policymakers with a set plan of action for achieving dementia risk reduction goals.” (10)
The bottom line:
Genetics is a factor, but how you live is the biggest factor in your well-being.
Lifestyle Medicine and Aging
Take a look at this picture:
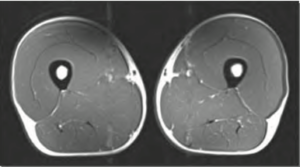
This is a magnetic-resonance-imaging scan of a 40-year-old man’s thigh. Note the thick muscles and thin layer of fat.
Take a look at this picture:
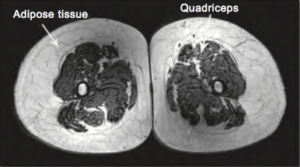
This is a scan of a 74-year-old man’s thigh. Note the significantly atrophied muscles and thick layer of fat.
Many people think this is simply what happens as they age. That is, they think “falling apart” is part of aging.
Take a look at one more picture:
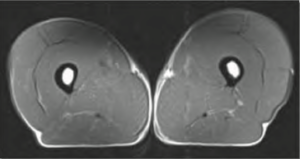
As you can see, this scan looks very similar to the first scan.
You might want to sit down for what I’m going to tell you now.
This is a scan of a 70-year-old-man’s thigh.
What the 40-year-old man whose thigh is shown in the first scan and the 70-year-old man whose thigh is shown in the third scan have in common is they both consistently exercised for years leading up to their scans. The man whose thigh is shown in the second scan was sedentary for years leading up to his scan.
These scans are from a scientific study with results published in The Physician and Sportsmedicine. Here’s how the researchers summarized their findings:
“The loss of lean muscle mass and the resulting subjective and objective weakness experienced with sedentary aging imposes significant but modifiable personal, societal, and economic burdens. As sports medicine clinicians, we must encourage people to become or remain active at all ages. This study, and those reviewed here, document the possibility to maintain muscle mass and strength across the ages via simple lifestyle changes.”
“This study contradicts the common observation that muscle mass and strength decline as a function of aging alone. Instead, these declines may signal the effect of chronic disuse rather than muscle aging. Evaluation of masters athletes removes disuse as a confounding variable in the study of lower-extremity function and loss of lean muscle mass. This maintenance of muscle mass and strength may decrease or eliminate the falls, functional decline, and loss of independence that are commonly seen in aging adults.”
“It is commonly believed that with aging comes an inevitable decline from vitality to frailty. This includes feeling weak and often the loss of independence. These declines may have more to do with lifestyle choices, including sedentary living and poor nutrition, than the absolute potential of musculoskeletal aging. In this study, we sought to eliminate the confounding variables of sedentary living and muscle disuse, and answer the question of what really happens to our muscles as we age if we are chronically active. This study and those discussed here show that we are capable of preserving both muscle mass and strength with lifelong physical activity.” (11)
We can extend this idea in very powerful ways.
If exercise can so powerfully maintain muscle and strength, what’s possible when a person meets most of their needs most of the time? And what’s possible for the other systems of their body?
What’s possible?
Absolutely thriving is what’s possible!
One beautiful thing about lifestyle medicine is that it adds years to your life and life to your years. It enables you to keep doing what you love to do well into your older years.
Meeting Your Needs
What does it mean to meet your needs?
These are the core behaviors that generally help people thrive:
- Eating well
- Exercising moderately
- Getting plenty of sleep
- Getting plenty of rest
- Engaging in fulfilling work
- Engaging in fulfilling relationships
An expanded list that includes some additional behaviors many people find helpful looks like this:
- Eating well
- Exercising moderately
- Getting plenty of sleep
- Getting plenty of rest
- Engaging in fulfilling work
- Engaging in fulfilling relationships
- Spending time with nature
- Experiencing solitude
- Creating and taking in art
- Employing relaxation techniques
- Participating in a spiritual practice
This might not all apply to you, and anything else you consider self-care can also be helpful.
Reactive Intervention and Proactive Prevention
Lifestyle medicine is just as much a mindset as it is a set of behaviors.
We don’t have to go back too many generations to discover a time when the key to wellness was reactive intervention.
Years ago, people weren’t suffering with type-2 diabetes, cardiovascular disease, cancer, dementia, chronic neuromusculosketetal pain, anxiety, depression, and related ailments like they are today.
People used to primarily get sick by being in an accident, being born with a hereditary ailment, or catching an infectious ailment.
Until recently, most people just lived their lives and relied on medical professionals to help them when they got sick.
Many factors have significantly reduced the burden of accident-related ailments, hereditary ailments, and infectious ailments.
At the same time, food processing, sedentary jobs, and other factors have created the ideal conditions for the development of lifestyle ailments.
Lifestyle ailments are ailments that develop over time as a result of lifestyle, and they’re predominantly what plague people these days.
In fact, eighty-six cents of every dollar spent on medical care goes to the symptom management of ailments that are reversible and preventable via lifestyle improvement. (12)
Consider type-2 diabetes.
I don’t say this to be flippant, I say it to make a clear point:
No one falls down and breaks their type-2 diabetes. No one is born with type-2 diabetes. No one catches type-2 diabetes. People develop type-2 diabetes over time.
As such, reactive intervention isn’t very effective at helping people with type-2 diabetes.
Type-2 diabetes, cardiovascular disease, cancer, dementia, chronic neuromusculosketetal pain, anxiety, depression, and related ailments require a different mindset: proactive prevention.
More and more people are realizing they can take control of their well-being. They’re realizing they can proactively start taking better care of themselves right away. They’re realizing they can learn to proactively meet most of their needs most of the time and thrive.
Lifestyle medicine is proactive prevention.
Lifestyle Medicine Is Empowering
Among the side benefits of lifestyle medicine is empowerment that spills into all areas of your life. Lifestyle medicine gives you an opportunity to take control of your well-being.
Let’s say a person has struggled with their eating habits for 20 years, and they’re struggling with their blood-sugar levels, blood pressure, blood-cholesterol levels, and/or weight.
Let’s say they start working on improving their eating habits. A month later, their metabolic biometrics are starting to improve, and they’ve lost six pounds. They have an incredible feeling: I did that! I’m doing this!
They think to themself, “If things are getting better because I’m eating better, what would happen if I added some exercise?” Then, they do just that. A month later, their blood pressure is approaching its optimal range, their blood-sugar and blood-cholesterol levels are continuing to improve, and they’ve lost 14 pounds. That incredible feeling is growing: I did that! I’m doing this!
Before they thought their well-being was declining because of “bad genes” and “getting older”. Now they realize they have a lot more power than they thought.
This sense of empowerment tends to spill out into all areas of a person’s life.
As a person gains confidence they can eat better and exercise more and greatly influence their well-being, they often start thinking about how they can meet more of their needs. They often start thinking about how they can get more sleep and rest. They often start thinking about how they can make their work and relationships more fulfilling.
Over time, they often make big improvements to many areas of their life.
There’s no stopping what an empowered person can do.
Alex
Most of my clients significantly improve their well-being, but one particular gentleman I worked with stands out as an example of the power of lifestyle medicine.
When Alex, a financial adviser and father of three, came to me, he was in his mid-50s. In his words, he was “feeling like crap”. He had pain in his shoulders, back, hips, and feet. He was tired all the time. All of his metabolic biometrics were going in the wrong direction, and he wanted to lose weight.
Here are the medical standards for several metrics along with Alex’s data before lifestyle improvement:
The medical parameters for body-mass index are:
- Underweight: < 18.5 body-mass index
- Normal: 18.5 to 24.9 body-mass index
- Overweight: 25 to 29.9 body-mass index
- Obese: ≥ 30 body-mass index
- Class 1 obesity: 30 to 34.9 body-mass index
- Class 2 obesity: 35 to 39.9 body-mass index
- Class 3 obesity: ≥ 40 body-mass index
Alex before lifestyle improvement: 35.3 body-mass index
The medical parameters for men’s waist circumference are:
- Low risk: ≤ 37 inches
- Intermediate risk: 37.1 to 39.9 inches
- High risk: ≥ 40 inches
Alex before lifestyle improvement: 38.5 inches
The medical parameters for hyperglycemia are:
Fasting-plasma-glucose test:
- Normal: < 100 milligrams per deciliter
- Prediabetes: 100 to 125 milligrams per deciliter
- Type-2 diabetes: ≥ 126 milligrams per deciliter
Alex before lifestyle improvement: 226 milligrams per deciliter
Glycated-hemoglobin test:
- Normal: < 5.7 percent
- Prediabetes: 5.7 to 6.4 percent
- Type-2 diabetes: ≥ 6.5 percent
Alex before lifestyle improvement: 9.5 percent
The medical parameters for hypertension are:
- Normal: < 120/80 millimeters of mercury
- Elevated: 120 to 129 systolic and < 80 diastolic millimeters of mercury
- Stage 1: 120-139/80-89 millimeters of mercury
- Stage 2: ≥ 140/90 millimeters of mercury
- Hypertensive crisis: systolic over 180 or diastolic over 120 millimeters of mercury
Alex before lifestyle improvement: 138/88 millimeters of mercury
The medical parameters for dyslipidemia are:
- Total cholesterol: < 200 milligrams per deciliter is optimal
- Low-density-lipoprotein cholesterol: < 70 milligrams per deciliter is optimal
- High-density-lipoprotein cholesterol: > 60 milligrams per deciliter is optimal
- Triglycerides: < 150 milligrams per deciliter is optimal
Alex before lifestyle improvement:
- Total cholesterol: 210 milligrams per deciliter
- Low-density-lipoprotein cholesterol: 127 milligrams per deciliter is optimal
- High-density-lipoprotein cholesterol: 36 milligrams per deciliter
- Triglycerides: 236 milligrams per deciliter
The medical parameters for metabolic syndrome are:
At least three of the following five risk factors:
- Waist circumference ≥ 40 inches (men) or ≥ 35 inches (women)
- Fasting plasma glucose ≥ 100 milligrams per deciliter
- Blood pressure ≥ 130/85 millimeters of mercury
- High-density-lipoprotein cholesterol < 40 milligrams per deciliter (men) or < 50 milligrams per deciliter (women)
- Triglycerides ≥ 150 milligrams per deciliter
Before lifestyle improvement, Alex met the standard for all of these risk factors except waist circumference.
Alex knew he had his work cut out for him. That didn’t stop him. He started by taking what is often the most important step in a person’s wellness journey: He got started.
Over time, by improving his eating habits, exercise habits, and other self-care habits, Alex made major improvements.
Eleven months into his wellness journey, this is what Alex’s numbers looked like:
Alex before lifestyle improvement: 35.3 body-mass index
Alex after lifestyle improvement: 26.4 body-mass index
Alex before lifestyle improvement: 38.5 inches (waist circumference)
Alex before lifestyle improvement: 32.5 inches (waist circumference)
Alex before lifestyle improvement: 226 milligrams per deciliter (fasting-plasma-glucose test)
Alex after lifestyle improvement: 94 milligrams per deciliter (fasting-plasma-glucose test)
Alex before lifestyle improvement: 9.5 percent (glycated-hemoglobin test)
Alex after lifestyle improvement: 4.9 percent (glycated-hemoglobin test)
Alex before lifestyle improvement: 138/88 millimeters of mercury (blood pressure)
Alex before lifestyle improvement: 123/78 millimeters of mercury (blood pressure)
Alex before lifestyle improvement:
- Total cholesterol: 210 milligrams per deciliter
- Low-density-lipoprotein cholesterol: 127 milligrams per deciliter is optimal
- High-density-lipoprotein cholesterol: 36 milligrams per deciliter
- Triglycerides: 236 milligrams per deciliter
Alex after lifestyle improvement:
- Total cholesterol: 188 milligrams per deciliter
- Low-density-lipoprotein cholesterol: 117 milligrams per deciliter is optimal
- High-density-lipoprotein cholesterol: 64 milligrams per deciliter
- Triglycerides: 139 milligrams per deciliter
At that point, Alex no longer met the standard for any of the risk factors for metabolic syndrome.
And he was absolutely full of energy. He told me he “felt like he was 25 again”. He used his newfound well-being to do more of what he loved to do like play golf, hike, go to concerts, and travel. He still had occasional aches and pains, but his joints felt a lot better. He told me his previous unwellness was like a “wet blanket that made everything harder”. He told me the best things about his newfound well-being were feeling like he could do whatever he wanted to do and the peace of mind that came with his improved outlook about his future.
I’m hesitant to tell you what Alex did to improve his well-being because I don’t want you to think of it as a prescription for you, but I also don’t want to leave you hanging. We’re all unique, so there isn’t one formula for improving wellness that works for all of us. With that in mind, here’s an overview of what Alex did:
- Over time, he shifted his food intake from about 25 percent real food and 75 percent junk food to about 90 percent real food and 10 percent junk food.
- Over time, he went from hardly exercising at all with the exception of very occasionally playing golf and hiking to consistently exercising four times a week (a combination of strength training and walking) along with playing golf and hiking whenever he could.
- He gradually improved his sleep hygiene and improved both the quantity and quality of his sleep.
- He went from someone who worked about 60 hours a week to someone who got some high-quality rest most days, took weekends off, and took vacations.
- He gradually streamlined his business by cutting out work he was doing out of obligation and doing more work he truly enjoyed and truly helped people.
- He leaned into his relationships big time.
- He made spending time with nature more of a priority because it helped him relax.
- He reprioritized his spiritual practice.
Again, each of us is unique. This is what worked for Alex. What will work for you depends on your unique needs.
One thing to highlight is Alex didn’t go on a radical diet or start doing a massive amount of exercise. He made significant improvements, but he didn’t do anything extreme.
Another thing to highlight is Alex took a holistic approach. There’s more to wellness than exercise and nutrition. Reducing stress and increasing fulfillment go a long way.
Finally, Alex didn’t do this overnight nor did it take him “forever”. He gradually made doable lifestyle improvements that worked for him and gradually cultivated practices he could make part of his life in lasting ways.
Your wellness journey will be your wellness journey. It won’t be Alex’s, but what Alex can do, you can do.
(1) Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population. Circulation, 2018, 10.1161/CIRCULATIONAHA.117.032047.
(2) Association Between Ultraprocessed Food Consumption and Risk of Mortality Among Middle-Aged Adults in France. JAMA Internal Medicine, 2019, 10.1001/jamainternmed.2018.7289.
(3) Fruit and Vegetable Consumption and Stroke: Meta-Analysis of Cohort Studies. The Lancet, 2006, 10.1016/S0140-6736(06)68069-0.
(4) Sedentary Lifestyle Associated with Mortality in Rural Patients with Heart Failure. European Journal of Cardiovascular Nursing, 2019, 10.1177/1474515118822967.
(5) Quantifying the Association Between Physical Activity and Cardiovascular Disease and Diabetes: A Systematic Review and Meta-Analysis. Journal of the American Heart Association: Cardiovascular and Cerebrovascular Disease, 2016, 10.1161/JAHA.115.002495.
(6) Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. The New England Journal of Medicine, 2002, 10.1056/NEJMoa012512.
(7) Association Between Physical Exercise and Mental Health in 1.2 Million Individuals in the USA Between 2011 and 2015: A Cross-Sectional Study. The Lancet Psychiatry, 10.1016/S2215-0366(18)30227-X.
(8) Social Relationships and Mortality Risk: A Meta-Analytic Review. PLOS Medicine, 2010, 10.1371/journal.pmed.1000316.
(9) Cancer Is a Preventable Disease That Requires Major Lifestyle Changes. Pharmaceutical Research, 2008, 10.1007/s11095-008-9661-9.
(10) Proportion of Dementia in Australia Explained by Common Modifiable Risk Factors. Alzheimer’s Research & Therapy, 2017, 10.1186/s13195-017-0238-x.
(11) Chronic Exercise Preserves Lean Muscle Mass in Masters Athletes. The Physician and Sportsmedicine, 2011, 10.3810/psm.2011.09.1933.
(12) Multiple Chronic Conditions Chartbook, Agency for Healthcare Research and Quality, 2014.
About Jason Gootman
Jason Gootman is a Mayo Clinic Certified Wellness Coach and National Board Certified Health and Wellness Coach as well as a certified nutritionist and certified exercise physiologist. Jason helps people reverse and prevent type-2 diabetes, cardiovascular disease, and other ailments with evidence-based approaches to nutrition, exercise, stress reduction, holistic wellness, and, most importantly, lasting behavior improvement and positive habit formation. As part of this work, Jason often helps people lose weight and keep it off, in part by helping them overcome the common challenges of yo-yo dieting and emotional eating. Jason helps people go from knowing what to do and having good intentions to consistently taking great care of themselves in ways that help them add years to their lives and life to their years.
Stay in the loop!
Subscribe today, and get wellness tips delivered straight to your inbox.